From simple case studies to double blind clinical trials, the many benefits of non-invasive imaging offers visual proof of treatment efficacy. Ultrasound in particular is more widely used to collect a patient's biometric data safely and efficiently, thanks to its vastly improved quantitative reporting capacity. Under exploratory device tech reviews, this video shows the effects of electromagnetic pulse waves neurostimulat stimulation and the induction of cold laser on the body are just some of the noninvasive modalities that are easily monitored with an ultrasound scan. In the case of electromagnetic devices, the involuntary muscle contraction is evidence of the electrical changes in the targeted muscle developers of this technology continue to find new evidence, supporting its ability to recover the body's process through cellular regeneration on a preliminary study, quantitative measurement that the regenerative timeline through the use of a neurostimulator through a simple before and after comparison can easily show the body's reaction to the therapeutic device. |
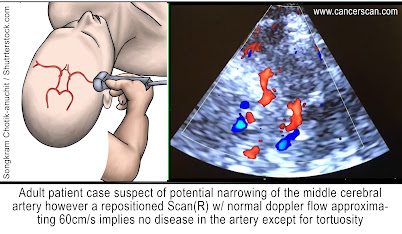
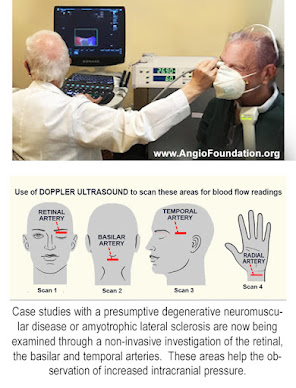
This case subject with a presumptive degenerative neuromuscular disease or amyotrophic lateral sclerosis. In a non-invasive investigation, we look at the eye for increased intracranial pressure, which may reflect in changes in the optic nerve diameter. [Fig. 1] The right eye, which is the left slide, shows the optic nerve diameter of five millimeters. And the right is almost eight millimeters. So we have a guide as to where the brain disease is more severe. At this point, we activate the blood flow function and look at the right eye and see that the blood flow from the anterior cerebral artery circulation that supplies the back of the eye is approximately 60 per second in the blood flow which corresponds to the graph on the bottom. [Fig. 2] On the left eye. The same blood vessel shows a decreased pressure of approximately 45 as shown by the decreased height of the blood flow graph at the bottom. Once again, we have measurable diagnostic technologies that are noninvasive, so we can follow treatment in diseases that are affecting the eye and as it relates to brain and degenerative neuromuscular disorders.
Now that radiologists are using Doppler blood flow to examine eye disease, including systemic diseases (including Diabetes, Brain tumors, heart disease, sickle cell disease etc) that affect the eye, we are hopeful that the ophthalmologic and neurological communities will start using this noninvasive technology as well to improve noninvasive and more rapid treatment of potential eye disorders, such as cancers of the eye, diabetes and glaucoma. Another future use will be to correlate the effect of decreased vascular pulsation in the production of cerebrospinal fluid that is removed by the cleansing glymphatic system is postulated as a contributing factor in degenerative neuromuscular disease.
Dr. Noelle Cutter (Biology professor and clinical researcher from Molloy College) joined with Dr. Robert L. Bard (top NYC radiologist and cancer diagnostic expert) to deploy the 2022 field study to provide breast screening to younger women, subjects with LOW BMI and those in underserved areas. "Through supplemental imaging (ie. 3D Doppler Ultrasound), we can provide better detection of tumors in dense breasts that are concealed by dense breast tissue from mammography."
Mammography is the current standard for breast cancer early detection for women 40 & older. Recent studies have shown nearly half of all women who get mammograms are found to have dense breasts, exposing this population to the risk that mammograms may miss potentially cancerous tumors concealed by dense breast tissue. Dr. Cutter's initial concepts to target LOW BMI (bet 12-22% body fat) was personally inspired. As an active TRIATHLETE, her own diagnosis sparked her survey and inquiry throughout the athletic community where she uncovered a significant trend that became the basis for this research. She wishes to target younger women, athletes and members of underserved communities. "Younger women may be more likely to have dense breasts... also I find athletes with LOWER BMI (body mass index) or those with less body fat are more likely to have more dense breast tissue compared with women who are obese." See full feature details |
Supplemental: DENSE BREAST DETECTION & IMAGE GUIDED ONCOLOGIC TREATMENT
In a recent clinical team effort between Dr. Robert Bard (cancer diagnostic imaging expert) and Dr. Jay Lombard, (an Integrative Neurologist), a multi-modal translational research program focused on the early detection and tracking of quantifiable biometrics of individuals suffering from neurodegenerative disorders. Based on prior/conventional diagnostic methods, Dr. Bard offers the integration of non-invasive innovations like the 3D Doppler Blood Flow Ultrasound imaging of the optic nerve and the Transcranial Doppler of the temporal artery to gather new and valuable data from the measurement of intercranial pressure and hemodynamics (vascular performance through blood flow readings) of the brain in various stages of the subject's condition. New findings from this program are directed to the support of optimizing research strategies leading to new treatment solutions.
(L) JAY LOMBARD, D.O. is a graduate of Nova Southeastern University of the Health Sciences where he received his Osteopathic Medical degree. He completed his Neurology residency at Long Island Jewish Medical and is the former chief of Neurology at Westchester Square Medical Center, Bronx Lebanon Hospital and adjunctive assistant clinical professor of Neurology. He is a published author of several peer reviewed articles on the pathogenesis of autism, Alzheimer's disease and autism. He has extensively lectured on the role of nutrition for the preservation of brain health and the importance of objective biomarkers for early detection of neurodegenerative diseases. He currently maintains a private practice in Valley Cottage, NY where he is primarily focused on Neurobehavioral and Neurodegenerative diseases.
(R) ROBERT L. BARD, MD paved the way for the study of various cancers both clinically and academically. Dr. Bard co-founded the 9/11 CancerScan program to bring additional diagnostic support to all first responders from Ground Zero. His main practice in midtown, NYC (Bard Diagnostic Imaging- www.CancerScan.com) uses the latest in digital Imaging technology has been also used to help guide biopsies and in many cases, even replicate much of the same reports of a clinical invasive biopsy. His most recent program is dedicated to the reporting of mental health diagnostic and innovative solutions including the use of modern neuromagnetic technologies and protocols.